kidney stones
KIDNEY STONES
Urinary tract stones form when urine becomes too concentrated with certain chemicals and substances that can turn into solids.
To make this clearer, think of salty water, which is full of sodium chloride, the chemicals that make up salt. When enough water is present, the salt remains dissolved in the water. But when the water evaporates, the residual salt solidifies at the bottom leaving the salt as a solid.
In the urinary tract, sodium chloride is not a problem, but other chemicals are. The most common chemical elements in stones are calcium, oxalate, phosphates and uric acid. Less common are magnesium, ammonia and cystine. Once a small stone has started, the urine tends to coat the small stone with more of the same chemicals, or sometimes other chemicals join in to make a complex stone. This is similiar to a piece of sand in an oyster. The sand is an irritant and the oyster coats the sand particle – and a pearl is formed!
CALCIUM STONES
By Boxing far the most common stones are made of a combination of calcium and oxalate. When calcium and oxalate join (or precipitate) they bind so tightly that most acids will not even dissolve them. Many foods, particularly dairy products, have calcium. Other foods such as spinach and green leafy vegtables are rich in oxalate. The body also manufactures its own oxalate, and the body stores immense amounts of calcium in the bones. Even if your diet has no calcium or oxalate, the urine will have some of these chemicals from the body stores. When too much calcium and oxalate join in the urine, a calcium oxalate stone can form. Other chemicals can join with calcium such as phosphate and carbonate to also form stones.
In the past, advice to patients who had suffered from calcium-containing kidney stones was to dramatically decrease the calcium in the diet, particularly milk and dairy products. We are not sure about that thinking today. A recently published medical study showed that those patients that took the highest amounts of calcium with their food were less likely to develop a stone over the next four years than those who consumed the smallest amount of the mineral! Just the opposite of what we have been telling people. The researchers speculated that calcium in the diet helped prevent the formation of kindey stones because it decreased the absorption of oxalate. Unattached (or free) oxalate, which is found in foods such as chocolate, spinach, colas, tea and peanuts is normally absorbed into the blood stream from the gut. As mentioned above, calcium oxalate together forms a very strong bond and calcium oxalate cannot be absorbed from the gut. Therefore if the oxalate can be bound to the calcium in the gut, it will not be absorbed. By maintaining an adequate amount of calcium in your diet you might decrease the oxalate absorption from the gastrointestinal tract and thus decrease the urinary excretion of oxalate.
There are also medications that can prevent calcium absorption from the gastrointestinal tract. Diuretics, such as hydrochlorothiazides, promote absorption of calcium from the kidneys and decrease the concentration in the urine.
URIC ACID STONES
After calcium containing stones, uric acid is the most common cause of stones comprising about 10% of the total number seen in the United States. Uric acid stones are very different from calcium stones. Uric acid is created within the body, it is not absorbed from the gut like calcium or oxalate. Uric acid comes from the breakdown of certain food products, particularly red meats. Uric acid does not need to join with another substance, it will form stones by itself. Uric acid forms in acid. The more acid the urine, the more precipitation of uric acid. Stones made of uric acid can be treated by two different methods, often combined together, reducing urine acidity and lowering the production of uric acid in the body. Lowering the acidity of the urine is accomplished by giving medications or chemicals which counteract acid (anti-acid) such as sodium bicarbonate or potassium citrate. A drug called allopurinol or Xyloprim decreases the production of uric acid in the body by blocking certain enzymes. Some patients with calcium oxalate stones will be found to have too much uric acid in their urine. We feel that many calcium stones form on smaller uric acid centers (similiar to a piece of sand causing a pearl in an oyster). By lowering the uric acid levels in the urine, these patients form fewer stones.
Uric acid is also responsible for gout and gouty arthritis, when too much uric acid is found in the joints. Not all patients with gout get uric acid stones and visa versa.
WATER INTAKE
Whatever the cause of stones, drinking plenty of water prevents stone formation. This occurs for two reasons. First, water dilutes the urine, making all the chemicals less concentrated and less apt to precipitate. Second, the increased flow may encourage the small stones to pass spontaneously before they reach a size that will not pass easily. An adult should drink more in general. This means that one might have to get up once or twice a night to urinate and drink another glass of water. However, if stones are prevented, the time spent is worthwhile. One should produce about 2 quarts of urine a day to prevent stones from forming. In those who exercise or do heavy physical labor, even more water intake is necessary.
If you have any questions regarding kidney stones or what dietary modifications you should make, ask your physician. Metropolitan Urologic Specialists conducts a kidney stone management clinic twice each month. Please call our scheduling office for information on dates.
DOUBLE J STENT INSTRUCTIONS
What is a double J stent?
A double J stent is a soft tube that is placed during surgery. This tube has a curl at both ends designed to prevent the stent from moving down into the bladder or up into the kidney. Some stents have a string attached to them which exits from the urethra. Stents are placed in the ureter which is the tube that runs from the kidney to the bladder.
Why is a stent placed?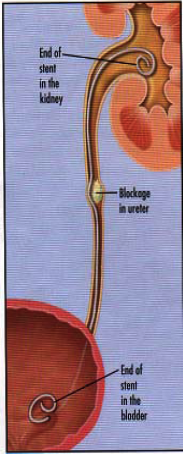
A stent is placed to prevent or relieve a blockage in the ureter. After many stone surgeries the small pieces of stone can drop down into the
ureter and block it, causing severe pain and occasionally infection. A stent allows the ureter to dilate, which makes it easier for stones or
stone fragments to pass.
Other surgeries in which stents are used includes:
- Removal of tumors from either the ureter or the kidney
- Repair of scars in the ureter
- Removal of tumors from around the ureter
What does it feel like to have a stent in your ureter?
The stent opens up the valve that prevents urine backing up into the kidney from the bladder when you urinate. This means that when you urinate, especially at the end, you may feel a slight tugging or stretching sensation in your back. If someone is very skinny or has very large back muscles, the stent sometimes can push on a nerve lying in the back of the abdomen, producing a temporary burning sensation in theback or in the upper thigh.
Most people will have some bladder irritation, especially at the end of urination. Often there is some frequency and burning with urination.
The stent can scratch the bladder lining so a small amount of bleeding can be expected either from the stent or the operation for which the stent was needed. Try to force fluids to flush out the bladder. Drink enough fluid to keep the urine watermelon colored or clearer. This bleeding may last as long as the stent is in place.
What can be done to treat the symptoms?
If you are having nerve irritation, try to decrease your activity, soak in a warm bath and take pain medication.
Should you have problems with urinary urgency, frequency and/or bladder discomfort, there are several medicines that we can give you:
- Pyridium is a bladder anesthetic that will decrease irritation from the stent. This medicine makes the bladder less sensitive. It normally turns the urine a deep pumpkin orange. This medicine is taken three times a day on an as-needed basis.
- If bladder spasms are severe, or you are bothered by severe urinary frequency or urgency, you may take a bladder-relaxant medicine such as Detrol or Ditropan. They do have side effects of dry mouth, constipation, dry eyes and occasional difficulty emptying the bladder out. If these side effects are too bothersome, stop the medicine. Should the side effects be less bothersome, cut the dose of medicine in half.
How long do I need to keep the stent in?
Stents are left in for varying lengths of time depending upon the reason for which the stent was placed. Talk to your doctor about how long you can expect to have to keep your stent. Stents usually are not left in for longer than three (3) months. IF YOUR STENT HAS BEEN LEFT IN FOR LONGER THAN 3 MONTHS, CONTACT YOUR UROLOGIST.
How are stents removed?
Stents with a string attached are pulled out gently by the patient, nurse or doctor. Stents without strings are removed in the urologist’s office by using a cystoscope to look in the bladder. It is recommended to drink 2 – 3 cups of fluid immediately after the stent is removed. You can expect some pain in the side or lower abdomen; some burning with urination and some blood in the urine for 2 – 3 days after the stent is removed.
When should the doctor be called?
- Rarely the stent may move down into the urethra tube. When this happens, urine leaks out continually as a steady drip.
- If you experience a fever of 101.0 degrees
ESWL Preoperative Patient Instructions
ONE WEEK BEFORE THE PROCEDURE:
Do not take aspirin (Bufferin, Excedrin, etc) or aspirin-containing medications such as Ibuprofen (Motrin, Nuprin or Advil), Indocin or Persantine (Dipyridamole). If you are taking aspirin or Persantine for your heart or to prevent stroke, check with your family doctor. If
you are taking any blood thinners (anticoagulants), such as Coumadin, please notify the prescribing physician.
THE DAY BEFORE THE PROCEDURE (SURGERY BEFORE 3 P.M.)
- Low fiber breakfast and lunch.
- At 3:00 p.m., drink one bottle (10 ounces) of Magnesium Citrate (purchased at your local drugstore) followed by at least 10 ounces of water or other liquids (except dairy products). You will probably have diarrhea for about two hours after this.
- Drink plenty (at least three glasses) of liquids (but not solid food) in the afternoon and evening.
- Liquids only (except dairy products) for dinner. This may be clear soups, jello, fruit juice, tea, coffee or sodas.
- Nothing to eat or drink after midnight unless otherwise instructed by your physician’s office/hospital. No smoking for 24 hours prior to surgery. You may rinse your mouth for tooth brushing.
THE DAY BEFORE THE PROCEDURE (SURGERY AFTER 3 P.M.)
- Low fiber lunch and dinner.
- At 7:00 p.m., drink one bottle (10 ounces) Magnesium Citrate (purchased at your local drugstore) followed by at least 10 ounces of water or other liquids (except dairy products). You will probably have diarrhea for about two hours after this.
- Drink plenty of clear fluids (at least three glasses) during the evening. The Morning of the Procedure (Surgery after 3 p.m.)
- You may have clear liquids only for breakfast (except dairy products) at least eight (8) hours prior to your procedure time.
- Nothing to eat or drink after midnight unless otherwise instructed by your physician’s office/hospital. No smoking for 24 hours prior to surgery. You may rinse your mouth for tooth brushing.
